Common Myths and Misconceptions About Actinic Keratosis
5 Actinic Keratosis Myths Debunked by a Dermatologist
 Prolonged exposure to sunlight is the primary cause of actinic keratosis, a common skin condition characterized by scaly, rough patches. These patches often appear on the face, hands, neck, and scalp. Over time, actinic keratosis lesions may enlarge, become itchy, or even disappear.
Prolonged exposure to sunlight is the primary cause of actinic keratosis, a common skin condition characterized by scaly, rough patches. These patches often appear on the face, hands, neck, and scalp. Over time, actinic keratosis lesions may enlarge, become itchy, or even disappear.Although actinic keratosis is not cancerous, misconceptions about this skin condition often deter people from seeking medical advice. It is crucial to have Actinic Keratosis and other skin abnormalities evaluated promptly by a dermatologist.
Read below to uncover the 5 common myths associated with Actinic Keratosis.
Myth 1: Actinic Keratosis Isn't Melanoma
Myth 2: Actinic Keratosis Is Just Age Spots, and Only Affects Older Adults
Age spots, on the other hand, are caused by increased melanin production due to sun exposure, resulting in darker skin patches.
Myth 3: Once an Actinic Keratosis Lesion Disappears, It Won’t Return
Sunscreen Recommendations
Myth 4: Wearing Sunscreen Prevents Actinic Keratosis
While sunscreen can reduce the risk of sunburn, mole growth, and Actinic Keratosis, it cannot entirely prevent sun damage. Using sunscreen with an SPF of at least 30 can reduce the number of new Actinic Keratosis lesions by up to 50% in one year. Wearing protective clothing, such as long-sleeve shirts, wide-brimmed hats, and long pants, is also essential for protecting your skin from UV rays.
Myth 5: Myth: Actinic Keratosis Can Be Treated with Non-prescription Products
Over-the-counter moisturizers may soften Actinic Keratosis lesions and improve texture, but they cannot treat Actinic Keratosis. Dermatologists often prescribe topicals such as Fluorouracil (5-FU) and Diclofenac to destroy precancerous cells in Actinic Keratosis lesions. Photodynamic therapy and cryotherapy are also effective treatments for Actinic Keratosis.
Importance of Regular Dermatological Check-Ups
Regular check-ups with a dermatologist are essential for early detection and treatment of actinic keratosis. Dermatologists can monitor your skin for changes and recommend appropriate treatment plans. If you have a history of actinic keratosis or extensive sun exposure, schedule annual skin examinations to catch potential problems early.
Visit Pinnacle Dermatology for Evaluation of Actinic Keratosis
Given the potential for actinic keratosis to develop into squamous cell carcinoma, Pinnacle Dermatology urges you to schedule an appointment for assessment and treatment of Actinic Keratosis lesions. Our dedication to maintaining healthy skin and enhancing the quality of life for our patients has established us as one of the leading dermatological centers nationwide
Featured Products for Sun Safety

EltaMD UV Clear SPF 46
Oil-free EltaMD UV Clear helps calm and protect sensitive skin types prone to discoloration and breakouts associated to acne and rosacea. It contains niacinamide (vitamin B3), hyaluronic acid and lactic acid, ingredients that promote the appearance of healthy-looking skin. Very lightweight and silky, it may be worn with makeup or alone. Choose from tinted and untinted formulas for use every day. 1.7 oz / 48 g

EltaMD UV Elements SPF 44 Tinted
EltaMD UV Elements is a 100% physical sunscreen in a tinted, moisturizing base. It is gentle for even the most sensitive skin types, including post-procedure skin. Its chemical-free actives, zinc oxide and titanium dioxide, provide safe but sure sun protection. These mineral-based UV filters work with ultra-hydrating hyaluronic acid to protect and hydrate the skin. UV Elements has a universal tint that beautifully enhances most skin tones for a more youthful appearance. 2 oz / 57 g
Featured Blogs

- Skin Cancer
- General Dermatology
- Skin Exams
Your skin is your largest organ and its first line of defense. Learn more about why a skin exam should be a part of your wellness routine.
Read More
- Skin Cancer
- Sun Safety
The sun's ultraviolet (UV) radiation poses a significant risk. Discover ways to protect you and your loved ones from the sun and keep your skin healthy all year long.
Read More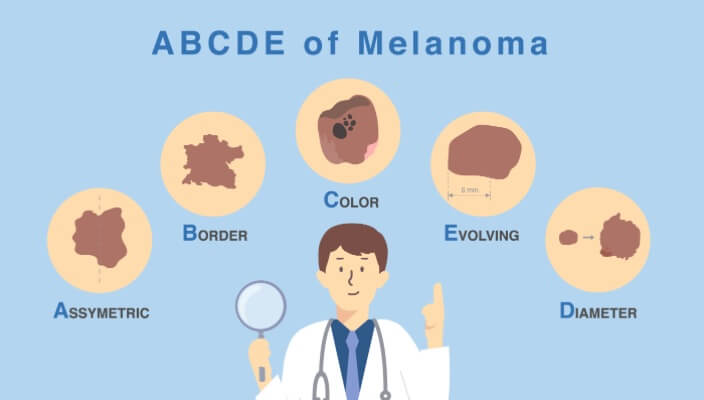
- Skin Cancer
- General Dermatology
- Skin Exams
Learn the ABCDEs of Melanoma, the deadliest form of skin cancer.
Read More


